 ISSN : 1598-2939
ISSN : 1598-2939
ⓒ Korea Institute of Sport Science
The study investigated the effects of hyperbaric oxygen therapy (HBOT) on ankle functions of patients with grade I ankle sprains. Two male patients with grade I acute ankle sprain were categorised into either combined HBOT and physiotherapy or physiotherapy only groups. Pain index and ankle isokinetic peak torque, time to peak torque and average power were evaluated on the first day of the injury before the commencement of the therapy and after a week of the therapy. The HBOT was administered with 2.5 ATA, 60 min per session, a session per day for five consecutive days. Standard physiotherapy was prescribed for both patients for a week. The data were analysed by descriptive statistics and percentage differences. Combined HBOT and physiotheraphy treatment was more effective in reducing pain compared to physiotherapy only. Isokinetic ankle strength improved in both patients from pre-test to post-test. However, the patient administered with combined HBOT and physiotherapy showed a higher percentage difference in isokinetic peak torque and time to peak torque compared to the other patient. Additional HBOT over the standardised physiotherapy in patient with grade I ankle sprain may help in reducing the pain sensation quicker, eliciting faster recovery, and improving isokinetic ankle strength.
The study investigated the effects of hyperbaric oxygen therapy (HBOT) on ankle functions of patients with grade I ankle sprains. Two male patients with grade I acute ankle sprain were categorised into either combined HBOT and physiotherapy or physiotherapy only groups. Pain index and ankle isokinetic peak torque, time to peak torque and average power were evaluated on the first day of the injury before the commencement of the therapy and after a week of the therapy. The HBOT was administered with 2.5 ATA, 60 min per session, a session per day for five consecutive days. Standard physiotherapy was prescribed for both patients for a week. The data were analysed by descriptive statistics and percentage differences. Combined HBOT and physiotheraphy treatment was more effective in reducing pain compared to physiotherapy only. Isokinetic ankle strength improved in both patients from pre-test to post-test. However, the patient administered with combined HBOT and physiotherapy showed a higher percentage difference in isokinetic peak torque and time to peak torque compared to the other patient. Additional HBOT over the standardised physiotherapy in patient with grade I ankle sprain may help in reducing the pain sensation quicker, eliciting faster recovery, and improving isokinetic ankle strength.
Ankle sprain is one of the most common sports-related injuries with an incidence rate of 60.9 per 10,000 individuals per year in the world (Hootman et al., 2007). Sports that register the highest incidence of ankle sprains are those requiring sudden stops and pivoting such as soccer, volleyball, and basketball (Eisenhart et al., 2003). These specific movements often result in ankle inversion during plantar flexion, which is the most common cause of ankle sprain. For high-performance athletes, ankle sprain not only limits their activities but also generates financial consequences due to their absence from participation (Lynch et al., 1999). The primary cost related to injury is the time lost from participating in sports which has compelled health care professionals to seek rapid and effective therapeutic interventions in treating ankle sprain and avoiding re-injury.
Grade I ankle sprain involved slight stretching and damage to the fibres of ankle ligaments that causes inflammation, swelling, bleeding and pain around the joint (Brostrom, 1966). Common treatment for grade I ankle sprain is rest, ice application, compression and elevation of the injured area (RICE). The sprained ankle is rested by limiting weight bearing activities and using crutches. Ice is applied to reduce the swelling (van den Bekerom et al., 2013). Compression using an elastic cloth bandage or athletic ankle braces helps to control swelling and add stability while the ligaments are healing (Lynch & Renstrom, 1999). The injured foot is elevated by reclining it up above the waist. Finally, rehabilitation is carried out to strengthen the ligament so that recurrence of the sprain may be avoided (Selvanetti et al., 2001).
Rehabilitation of ankle sprain should include passive joint mobilisation to reduce pain and increase range of motion of the injured joint (Landrum et al., 2008). The joint mobilisation should be done as early as two days post injury for better prognosis and reduce risk of injury recurrence (Eiif et al., 1994). Ankle sprain causes edema and ligament tear which may further lead to muscle damage in nearby area (Donovan & Hertel, 2012). Therefore, passive strain exercise was suggested to strengthen the injured muscle. Strengthening of weakened muscles was essential for rapid recovery and prevention against re-injury (Thacer et al., 1999). Strengthening the injured muscle begins with isometric exercises performed against an immovable object and progresses to dynamic resistive exercises using ankle resistance band, which is similar to towel stretches strain exercise (Mattacola & Dwyer, 2002).
Hyperbaric oxygen therapy (HBOT) may provide an alternative means of therapy to facilitate a speedier resumption to pre-injury activity levels through the administration of pure oxygen at pressures greater than atmospheric pressure (Babul & Rhodes, 2000). Studies have shown that HBOT can reduce edema through vasoconstriction which decreases blood flow to the injured area (Davidkin, 1977). Specifically in sports-related injuries, HBOT was conducted on an ankle injuries study where the patients exposed to HBOT returned to sports activity 30% faster than the control group (James et al., 1993). Borromeo et al. (1997) also reported that patients with acute ankle sprains who were administered with HBOT (100% oxygen at 2 ATA for 90 min for the first session and 60 mins for the other two sessions) had improved joint function compared to the control group who were exposed to ambient air (1.1 ATA for 90 min). Another clinical study examining the short term recovery of grade II medial collateral ligament injuries of the knee indicated that recovery was more rapid in the HBOT exposed patients compared with the control group (Soolsma, 1996). Despite the advantages of HBOT, studies regarding its effects on ankle sprain are scarce and dated, particularly on the objective measurement of isokinetic ankle strength following the therapy. Therefore, the purpose of this case study was to compare the effects of combined HBOT and physiotherapy and physiotherapy only on pain sensation, isokinetic peak torque, isokinetic time to peak torque and average power of patients with grade I ankle sprains.
Participation in the present study was entirely voluntary. All procedures were conducted at Universiti Sains Malaysia (USM) in compliance with the Helsinki Declaration of 1975. Ethical approval was obtained from the Human Research Ethics Committee of USM (USM/JEPeM/15040122). The study only included patients with an age range between 18-50 years old and, with confirmed grade I ankle sprain of the lateral collateral ligament. The clinical examination was conducted by an orthopedic specialist at the Emergency Department of Hospital Universiti Sains Malaysia (HUSM) which included inspection, palpation, testing of ankle joint laxity and instability in the frontal and sagittal plane. The patients were prescribed with RICE (rest, ice, compression, elevation) treatment.
Patients with complete rupture (grade II and grade III) of the lateral collateral ligament and any lower limb fracture were excluded. Patients with contraindications for HBOT such as pulmonary disease, severe asthma, active allergies, upper respiratory infection, epilepsy, or claustrophobia were also excluded. The patients were randomly assigned into either receiving combined physiotherapy and HBOT or physiotherapy only.
The anthropometric parameters such as body height, body weight, body composition and blood pressure were measured at pre-test. A portable stadiometer (Seca 220, Germany) was used to measure the height of the patients. The body weight and body composition were measured by using Body Composition Analyzer (TANITA, model TBF-410, Japan). During the measurement, the patients were asked to take off their footwear and wore light clothing. Blood pressure was measured using an automated blood pressure monitor (A&D, Model TM-2540, Japan).
The level of pain at the time of examination was assessed using the Visual Analogue Scale. The scale was 10 cm long with 'no pain' at one end, and 'the most pain imaginable' at the other end. The patient was required to mark with a pen along the line to match the level of pain that he or she perceived. The distance marked along the line by the patient was calculated to the nearest mm. The pain scale was monitored daily during the treatment week.
During ankle functional test, both legs were tested for isokinetic strength using a dynamometer (Multi-joint System Biodex Pro, Shirley, NY, USA). The pre-test was conducted during the acute stage of injury while the post test was conducted following seven days of the treatment program. The patients were seated on the chair with a support pad placed under distal femur and secured with strap. Painless range of motion for ankle plantarflexion, dorsiflexion, eversion and inversion were evaluated. The patients were required to push to the best of their ability for 10s in the painless range of motion as determined previously. The velocity of the movement was set at 120°.s-1 as this velocity has been recommended for ankle sprain evaluation (Fugl-Meyer, 1981; Leslie et al., 1990). For ankle plantarflexion and dorsiflexion, movement started with dorsiflexion. For ankle inversion and eversion, movement started with eversion. Two consecutive trials for each tested motions were recorded.
The patient who was given the additional HBOT attended the hyperbaric oxygen chamber (Sigma Plus Monoplace Hyberbaric System Perry Baromedical Riviera Beach, FL, USA) therapy and followed by a standardised physiotherapy for ankle sprain prescribed by the local hospital whereas the control patient only followed the standardised physiotherapy.
For the hyperbaric oxygen therapy group, the patient was treated using 2.5 ATA for 60 min per session. Five sessions were conducted for five consecutive days. Prior to the HBOT, the patient was examined by a medical assistant and tested for the blood glucose level to ensure that he does not faint inside the chamber due to hypoxia or hypoglycaemia. When the patient entered the hyperbaric chamber, he was given 15 min to familiarise with the environment before ATA was increased. After 60 min of treatment at 2.5 ATA, the patient was given another 15 min of rest at normal ATA to familiarise with the decrease of the pressure back to normal condition. Following that, the patient was requested to exit from the hyperbaric chamber. The amount of ATA and total duration of HBOT sessions were greater than the previous studies (Borromeo et al., 1997; Wilson et al., 2007). Meanwhile, the standardised physiotherapy which was provided for one week included passive joint mobilisation and passive stretching exercises (Table 1).
|
RICE : Rest, Ice, Compression and Elevation Rest: ankle was rested by not walking on it, limit weight bearing on ankle or use crutches if necessary Ice: Apply ice to minimise swelling. 24-48 hr after injury. Apply for 10 to 15 minutes, 3 or more times a day Compression: Wrapping the injured or sore area with an elastic bandage to help decrease swelling Elevation: Elevate the injured or sore area on pillows while applying ice and anytime patients are sitting or lying down, recommended to apply during sleep. Keep the area at or above the level of heart to help minimize swelling Passive joint mobilisation Stretch exercise with towels: hold for 15-30 seconds, 10-20 repetitions, 3-4 times a day, after 72 hours of pain One-leg stance balance exercise: hold for 20-30 seconds, 10 repetition, 3-4 times a day (perform when subject can ambulate pain-free on a leveled surface without assistive device) |
Pain index and isokinetic ankle strength of the patients were compared. Percentage differences between pre-test and post-test in isokinetic variables were determined using the formula below:
The characteristics of the two patients are presented in Table 2. The ankle sprains occurred during recreational sports and the patients did not have any previous ankle sprains greater than first degree or fracture in the ankle joint. Both patients were medically examined through a standard procedure by an orthopedic specialist and had been confirmed with grade I lateral ankle sprain.
| HBOT & Physiotherapy | Physiotherapy | |
|---|---|---|
| Age (year) | 24 | 35 |
| Gender | Male | Male |
| Weight (kg) | 90 | 83 |
| Height (cm) | 178 | 168 |
| BMI (kg.m-2) | 28.4 | 29.4 |
| Blood pressure (mmHg) | 133/73 | 130/78 |
| Body fat percentage (%) | 31.2 | 31.5 |
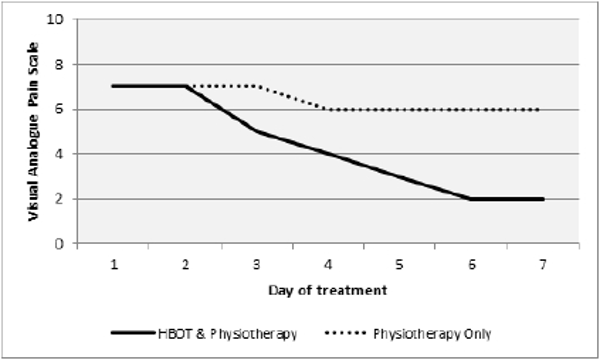
Daily evaluation of pain perception is shown in Figure 1. The patient who was given the additional HBOT had a lower pain score from day 2 onwards compared to the patient who was only given the standard physiotheraphy. The results of isokinetic peak torque, time to peak torque and average power of the ankle joint for dorsiflexion, plantarflexion, eversion and inversion were compared before and after treatment. The patient with HBOT plus physiotheraphy treatment had a higher percent difference in all the isokinetic parameters measured except for average power during eversion and inversion (Table 3, 4 and 5).
| Isokinetic Ankle Peak Torque (Nm) | HBOT & Physiotherapy | Physiotherapy |
|---|---|---|
| Dorsiflexion (Nm) Pre-test Post-test % difference |
16.5 (0.1) 27.3 (0.2) 65.1 |
14.6 (0.7) 16.2 (2.8) 10.9 |
| Plantarflexion (Nm) Pre-test Post-test % difference |
8.5 (0.2) 16.1 (0.1) 88.3 |
6.4 (1.7) 11.4 (4.1) 77.5 |
| Eversion (Nm) Pre-test Post-test % difference |
7.3 (0.9) 11.6 (0.4) 58.9 |
5.1 (1.2) 8.0 (0.4) 57.8 |
| Inversion (Nm) Pre-test Post-test % difference |
6.7 (0.7) 10.7 (0.7) 59.2 |
7.3 (1.5) 8.2 (0.7) 12.3 |
| Isokinetic Ankle Time to Peak Torque (ms) | HBOT & Physiotherapy | Physiotherapy |
|---|---|---|
| Dorsiflexion (ms) Pre-test Post-test % difference |
415.0 (35.3) 75.0 (7.1) -81.9 |
255.0(49.5) 225.0 (35.3) -13.3 |
| Plantarflexion (ms) Pre-test Post-test % difference |
565.0 (7.1) 220.0 (0.1) -61.1 |
385.0 (77.8) 185.0 (63.6) -51.9 |
| Eversion (ms) Pre-test Post-test % difference |
420.0 (0.1) 190.0 (7.1) -54.76 |
335.0 (134.4) 245.0 (7.1) -36.73 |
| Inversion (ms) Pre-test Post-test % difference |
465.0(35.4) 230.0(28.3) -50.5 |
430.0 (0) 300.0 (169.7) -30.2 |
| Isokinetic Ankle Average Power (W) | HBOT & Physiotherapy | Physiotherapy |
|---|---|---|
| Dorsiflexion (W) Pre-test Post-test % difference |
12.5 (0.6) 25.1 (0.3) 100.8 |
10.0 (0.1) 10.8 (0.3) 7.4 |
| Plantarflexion (W) Pre-test Post-test % difference |
4.3 (0.1) 10.6 (0.9) 146.5 |
2.6 (0.9) 5.4 (0.7) 107.7 |
| Eversion (W) Pre-test Post-test % difference |
3.5 (0.4) 9.9 (0.5) 181.4 |
2.0 (0.3) 6.1 (0.7) 202.5 |
| Inversion (W) Pre-test Post-test % difference |
5.2 (1.2) 7.4 (1.1) 42.7 |
2.9 (0.6) 6.2 (0.1) 117.5 |
In this case study, we found that HBOT was able to provide faster recovery of pain and ankle strength compared to standardised physiotherapy. The application of HBOT for the management of sports injuries has been recommended as a primary or an adjunct treatment modality (Babul et al., 2003). The healing of an injury follows a fairly consistent pattern irrespective of the underlying causes. The three phases identified in this process include the inflammatory phase, the proliferative phase and the remodelling phase. The presence of oxygen has an important role in each of these phases (Ishii et al., 2005). In the inflammatory phase, the hypoxia-induced factor-1a, which promotes the glycolytic system, vascularisation and angiogenesis, has been shown to be important. If the oxygen supply could be controlled without promoting blood flow, the blood vessel permeability could be controlled to reduce swelling and pain (Barata et. al., 2011). In the proliferative phase, the oxygen supply to the injured area is essential for the synthesis of extracellular matrix components such as fibronectin and proteoglycan (Barata et. al., 2011). In the remodelling phase, injured tissue is slowly replaced using the oxygen supply provided by the blood vessel Barata et. al., 2011).
The results of visual analogue pain scale showed that the HBOT was more effective in reducing pain compared to the control patient after seven days of intervention. We speculated that the effects were due to the decrease of inflammation and mechanical hypersensitivity of pain following HBOT as shown in previous animal study (Wilson et al., 2007).
Our finding was contrary to a previous study by Borromeo and colleagues (1997). They examined the effect of HBOT on ankle sprain within seven days of 2.0 ATA, with an initial treatment session which lasted 90 minutes and the remaining two treatments, 60 minutes. In comparison with placebo group, it was reported that the pain score for the treatment group was higher throughout the study although both groups showed significant pain reduction over the duration of treatment (Borromeo et al., 1997). The contradiction from our finding may be due to frequent sessions of 2.5 ATA by our patient. Hence, increasing the ATA and the frequency of HBOT session may enhance faster recovery from pain.
Using the similar visual analogue pain scale, it was reported that pain was relieved in five of the six chronic occlusive disease patients following HBOT (Urayama et al., 1992). Furthermore, six weeks of HBOT had positive effect on lowering the pain score of grade II tear of knee medial ligament (Soolsma, 1996). Besides, HBOT was shown to be effective in pain management in fibromyalgia syndrome (Yildiz et al., 2004), complex regional pain syndrome (Kiralp et al., 2004), delayed onset of muscle soreness (Staples & Clement, 1996), and headache (Di Sabato et al., 1996). Hence, the findings from our present study and previous researches reflected the effectiveness of HBOT in reducing pain.
Peak torque is the measurement of maximal ankle strength. Muscle strength plays an important role in ankle stability and muscle weakness may cause persistent instability of the ankle (Willems et al., 2002). Weakness of ankle joint muscles increases the risk of injury. Before treatment, the isokinetic ankle peak torque for plantarflexion of both patients was low due to ankle sprain. This is in agreement with other studies showing persistent weakness in plantarflexion in patients with lateral ankle sprain (Wilkerson et al., 1997). Our findings noted the increment of isokinetic ankle peak torque occurred following both types of treatment. Further analysis showed that the value of percentage difference of peak torque during ankle plantarflexion, dorsiflexion, eversion and inversion was greater in the patient who was treated with combined HBOT and physiotherapy compared to the patient who was treated with physiotherapy only. Among the tested ankle motions, the percentage difference of isokinetic ankle plantarflexion was the greatest following both treatments. This finding is important because natural recovery of ankle sprain showed that weakness of plantarflexors persisted even after 30 days post injury (Aiken et al., 2008). Furthermore, Staples and Clement (1996) showed that greater recovery of eccentric strength was achieved following treatment with HBOT at 2.0 ATA for five days compared to three days of HBOT and placebo. Therefore, it can be summarised that HBOT may promote recovery of eccentric strength in muscle, promote return to normal stiffness of the ligaments, and enhance recovery of ligament strength.
Time to peak torque is defined as the time from the start of muscular contraction to the point of highest torque development in a selected motion. It is an indicator of the functional ability to produce torque quickly and can be used to determine explosive power (Whipple et al., 1987). A prolonged time to peak torque indicates reduced recruitment of type II fibres (Kannus, 1994). Muscle damage in nearby area of a sprained ankle may further lead to muscle weakness and thus alter the time to peak torque. Our findings showed that the time to peak torque of ankle plantarflexion, dorsiflexion, eversion and inversion of the patient who underwent combined HBOT and physiotherapy decreased sharply from baseline value compared to the other patient. This result is in parallel with previous studies which showed that HBOT accelerated recovery from muscle damage (Babul et al., 2003), delayed onset of muscle soreness (Staples & Clement, 1996; Webster et al., 2002), and acute muscle stretch injury (Best et al., 1998).
Average power was included in the study to measure the rate of recovery. Muscle power of the ankle is the product of the force produced and the movement velocity (Newton & Kraemer, 1994). Reduced muscular power and movement velocity are associated with an increased probability of falls and a reduction in the ability to perform activities of daily living due to injury (Grabiner et al., 1993). The results from the present study showed that average power ankle plantarflexion, dorsiflexion, eversion and inversion increased from pre-test to post-test for both patients. This may be due to the ability to generate faster and greater torque following pain reduction. However, the results were contradictory to previous studies which did not show any evidence on the effect of HBOT on isokinetic average power (Babul et al., 2003; Barata et al., 2011). Furthermore, a study on the effects of HBOT on exercise-induced muscle soreness, observed that HBOT did not alter leg circumference, quadriceps peak torque, average power or fatigue compared to the control group, although faster recovery was observed in the HBOT group on third day of treatment (Germain et al., 2003). The contradiction may be caused by greater ATA and frequency of HBOT session exposed to our patient in conjuction of prescribed standardised physiotherapy.
Data from the present study demonstrated that combined HBOT and physiotherapy was more effective in reducing pain compared to physiotherapy only. In addition, the patient administered with HBOT has a higher percentage difference in isokinetic peak torque and time to peak torque compared to the control. Thus, we conclude that to enhance recovery from lateral ankle sprain grade I, HBOT can be prescribed as an additional treatment modality. Faster recovery may shorten the duration of absence from play due to injury which is a concern for professional athletes.
The authors are thankful to the participating patients. We thanked Associate Professor Dr Tengku Muzaffar Tengku Mohamad Shihabuddin from the Department of Orthopedics, School of Medical Sciences, Universiti Sains Malaysia, for consultation.
This project was financially supported by USM Research University Grant (Grant No: 1000/PPSP/812113).