Comparison of the effects of short-term stair climbing and walking exercise on vascular function in healthy young adults
International Journal of Applied Sports Sciences, Vol.30, No.2, pp.125-133
https://doi.org/10.24985/ijass.2018.30.2.125
© Korea Institute of Sport Science
초록
Stair climbing is a form of physical activity that can be easily accessible in worksites and public settings, but it remains unclear whether stair climbing exercise is more effective in improving vascular health than walking exercise. The aim of this study was to compare the short-term effects of stair climbing exercise and walking exercise on vascular function in healthy young adults. Eighteen healthy adults were randomized to either the stair climbing exercise group (n=10) or the walking exercise group (n=8). The stair climbing exercise was performed inside a building, while the walking exercise involved a brisk walking exercise on the treadmill at the same exercise intensity (50-60% of heart rate reserve) for 2 weeks, 30 min/day, and 3 times/week. Peak oxygen uptake was measured by maximal cardiopulmonary exercise test. Carotid-femoral pulse wave velocity (c-f PWV) and flow-mediated dilation (FMD) as indexes of vascular function were measured using applanation tonometry and ultrasound machine, respectively. These variables were measured at baseline and again after 2 weeks of supervised exercise in both groups. FMD improved similarly in both groups (stair climbing: 11.5±2.2 to 14.3±2.4%, walking: 10.8±1.3 to 12.1±2.9%, time effect: p<0.05). However, an improvement in c-f PWV did not reach statistical significance in both groups (stair climbing: 6.83±0.8 to 6.40±0.88 m/s, walking: 6.61±0.8 to 6.46±0.85 m/s, p=0.051). No changes in peak oxygen uptake were observed in any group (stair climbing: 35.47±7.83 to 37.03±8.26 mL/kg/min, walking: 37.46±5.21 to 38.33±6.73 mL.kg/min, p=0.726). These findings suggest that both short-term stair climbing and treadmill walking exercises were comparatively effective in improving conduit artery endothelial function in healthy young adults.
Abstract
Stair climbing is a form of physical activity that can be easily accessible in worksites and public settings, but it remains unclear whether stair climbing exercise is more effective in improving vascular health than walking exercise. The aim of this study was to compare the short-term effects of stair climbing exercise and walking exercise on vascular function in healthy young adults. Eighteen healthy adults were randomized to either the stair climbing exercise group (n=10) or the walking exercise group (n=8). The stair climbing exercise was performed inside a building, while the walking exercise involved a brisk walking exercise on the treadmill at the same exercise intensity (50-60% of heart rate reserve) for 2 weeks, 30 min/day, and 3 times/week. Peak oxygen uptake was measured by maximal cardiopulmonary exercise test. Carotid-femoral pulse wave velocity (c-f PWV) and flow-mediated dilation (FMD) as indexes of vascular function were measured using applanation tonometry and ultrasound machine, respectively. These variables were measured at baseline and again after 2 weeks of supervised exercise in both groups. FMD improved similarly in both groups (stair climbing: 11.5±2.2 to 14.3±2.4%, walking: 10.8±1.3 to 12.1±2.9%, time effect: p<0.05). However, an improvement in c-f PWV did not reach statistical significance in both groups (stair climbing: 6.83±0.8 to 6.40±0.88 m/s, walking: 6.61±0.8 to 6.46±0.85 m/s, p=0.051). No changes in peak oxygen uptake were observed in any group (stair climbing: 35.47±7.83 to 37.03±8.26 mL/kg/min, walking: 37.46±5.21 to 38.33±6.73 mL.kg/min, p=0.726). These findings suggest that both short-term stair climbing and treadmill walking exercises were comparatively effective in improving conduit artery endothelial function in healthy young adults.
Introduction
Cardiovascular disease (CVD) is the major cause of death worldwide. Emerging evidence has suggested that vascular dysfunction such as heightened arterial stiffening (Sutton-Tyrrell et al., 2005; Boutouyrie et al. 2002; Vlachopoulos et al., 2010) and impaired endothelial-dependent vasodilation (Yeboah et al., 2009; Inaba et al., 2010) are predictors of cardiovascular events, independently of traditional cardiovascular risk factors. Therefore, strategies aimed at improving vascular function are critical for the prevention of and treatment for CVD.
Increased physical activity is recommended as a lifestyle strategy to help reduce cardiovascular risk and improve vascular function (Ashor et al., 2014; Jungersten et al., 1997; Tanaka et al., 2000). Specifically, the American Heart Association and the American College of Sports Medicine have recommended a minimum of 30 minutes of moderate-intensity aerobic exercise, at least 5 days a week, for maintaining good health and preventing CVD (Haskell et al., 2007). Importantly, higher physical activity and fitness levels are associated with a lower risk of CVD mortality (Ashor et al., 2014; Laukkanen et al., 2016). Unfortunately, despite much effort put forth in establishing such physical activity guidelines (Haskell et al., 2007), many individuals still do not meet the current exercise recommendation due to lack of time and difficulty for accessing to exercise facilities (An et al., 2016). As such, alternative methods of increasing physical activity levels that are more easily accessible are warranted.
Interestingly, stair climbing may serve as an alternative form of exercise that is not only cost effective, but also more easily accessible in worksites and public settings (Moatari-Kazerouni et al., 2016; Bellicha et al., 2015). Compared with walking exercise, stair climbing requires more muscular demands, attributable to larger ranges of motion, forces, angles, and moments at the ankles, knees, and hip joints (Costigan et al., 2002; Andriacchi et al., 1980; McFadyen et el., 1988), so it is easy to increase exercise intensity with same speed. In addition, Stair climbing has been reported to improve maximal aerobic capacity, body composition, and muscular strength, as well as reduced low-density lipoprotein cholesterol (Boreham et al., 2005; Loy et al., 1994). Given the cardioprotective benefits of stair climbing, it would be worthwhile to explore the beneficial effects of stair climbing on vascular function, as this area of research is less well known. In particular, it remains unclear whether stair climbing may be as effective as walking exercise in improving vascular health. Previous studies found that 4-24 weeks of stair exercise training improves fitness and CVD risk factors (Loy et al., 1994; Boreham et al., 2005; Meyer et al., 2010). However, an even shorter duration of exercise training (6-10 days) has also been demonstrated to improve aerobic capacity, arterial stiffness, and glucose tolerance (Rogers et al., 1988; Baynard et al., 2009; Liu et al., 2015; Baykara et al., 2017). Importantly, such short-term training study designs are useful to determine and compare the effects of exercise training itself without the confounder such as weight loss.
Therefore, the purpose of this study was to compare the short-term effects of stair climbing vs. treadmill walking exercise at the same exercise intensity on vascular function in healthy young adults. We hypothesized that stair climbing would yield similar benefits on vascular function compared with walking exercise.
Methods
Study subjects and design
Twenty healthy young adults (male=10) volunteering for this study were recruited from the University of Seoul (UOS) through advertisements. Participants were randomized to either the stair climbing exercise group (n=10) or the walking exercise group (n=10). Written informed consent and standardized health questionnaire were obtained before study participation. Participants were sedentary and were not engaged in any regular exercise training program, and all were normotensive (systolic blood pressure (SBP) <140 mmHg and diastolic blood pressure (DBP) < 90 mmHg), non-obese, non-smoker, and free of any known cardiovascular or metabolic diseases. None were taking medications known to affect heart rate (HR) or blood pressure (BP), including anti-inflammatories. Female participants were studied during days 1-7 of their menstrual cycle or during the placebo pill phase, if on oral contraceptives. All measurements were performed in the morning after 8 or more hours of fasting at baseline and again after 2 weeks of exercise. Tests of after 2 weeks of exercise were conducted 20-24h after their last exercise training session to avoid the temporary effects of exercise. Participants were instructed to refrain from alcohol, caffeine, and exercise for 24h before study participation.
Exercise training protocol
Participants in both groups completed stair climbing exercise or walking exercise at moderate intensity (50~60% of heart rate reserve (HRR)) for 30 minutes, 3 days per week for 2 weeks. In the stair climbing exercise group, participants walked up one flight of stairs (17cm/22step), turned at the top of the stairs, and then walked back down the stairs. On the other hand, participants in the walking exercise group walked on a treadmill for the same of time at the same exercise intensity. HR was monitored using a wireless monitor device (RS800CX, Polar, Finland) to ensure the participants exercised at the prescribed exercise intensity. If HR fell below 50-60% of HRR, speed was the only variable that was adjusted during exercise in both groups.
Body composition and blood pressure measurements
Body mass index (kg/m2) and body fat (%) were obtained using the bioelectrical impedance analysis (Inbody 3.0, Biospace, South Korea). Brachial BP was measured in the supine position using automatic sphygmomanometer (HEM-7080IC, OMRON DALIAN CO., China), following at least 10 minutes of quiet rest. BP was taken twice, separated by 3 minutes, and the lower BP was used for analysis. In addition, radial pressure waveforms were obtained using applanation tonometry with a high-fidelity strain-gauge transducer (SphygmoCor, AtCor Medical, Sydney, Australia). Then, central SBP (CSBP) and DBP (CDBP) was derived from the radial BP waveforms using a generalized validated transfer function (Pauca et al., 2001).
Arterial stiffness measurement
Carotid-femoral pulse wave velocity (c-f PWV) as a biomarker of central arterial stiffness was measured in accordance with established guidelines (Van Bortel et al., 2012; Van Bortel et al 2001). The pressure waveforms were obtained for a 10-sec epoch from the right common carotid artery and the right femoral artery using a high-fidelity strain-gauge transducer (Millar Instruments, Houston, TX). The peak of an in-phase R wave, as obtained from sequential ECG monitoring (CM5 configuration) was used as a timing marker. The foot of the pressure wave was identified automatically to avoid any potential observer bias using an algorithm that detects the initial upstroke via a line tangent to the initial systolic upstroke point of the pressure tracing and an intersecting horizontal line through the minimum point (Bunsawat et al., 2017). The distances from the carotid artery to the suprasternal notch and from the suprasternal notch to the femoral artery were measured as straight lines using a tape measure. The distance was from the carotid artery to the suprasternal notch was then subtracted from the suprasternal notch-femoral artery segment to correct for differences in propagation direction along the arterial path (Bunsawat et al., 2017). This technique has been demonstrated to be highly reproducible (Wilkinson et al., 2002).
Endothelial function measurement
Endothelium-dependent vasodilation was assessed as flow-mediated dilation (FMD) of the brachial artery using ultrasonography (ACUSON X 300, Siemens, Mountain View, CA, USA), as previously described (Bunsawat et al., 2017; Solini et al., 2012). Briefly, following 1 minute of baseline data acquisition, the BP cuff was inflated on the participant’s right arm, approximately 2-4 cm distal to the antecubital fossa, for 5 minutes and then deflated to induce reactive hyperemia. The brachial artery was imagined in a longitudinal section, 5-10 cm proximal to placement of the BP cuff just below the antecubital fossa using a high-frequency (11.3 MHz) linear array probed. Brachial artery diameter was measured on acquired images using a computerized edge detection system (FMD studio, Quipu s.r.l., Pisa, Italy). FMD was calculated as the maximum percent increase in diameter above baseline following reactive hyperemia. All measurements were conducted by the same trained investigator.
Peak aerobic capacity measurement
Peak aerobic capacity (VO2peak) was measured by an open-circuit spirometry metabolic system (TrueOne 2400, Parvo Medics, Sandy, UT, USA) using the conventional Bruce treadmill protocol. VO2peak was defined as the highest or peak attained oxygen consumption, and was expressed as mL/kg/min. HR was measured every 3 minutes during and every minute after exercise using a continuous 12-lead ECG recording (Q-Stress, Quinton Q-4500, Bothell, WA, USA). The test was terminated when participants met 3 of the 5 following criteria (American College of Sports Medicine [ACSM], 2013): (1) a plateau in HR despite an increase in workload, (2) a plateau in oxygen uptake with an increase in workload, (3) ratings of perceived exertion ≥17 (scale 6-20), (4) the inability to maintain adequate pace to keep up with treadmill speed, and (5) a respiratory exchange ratio ≥1.1.
Statistical analysis
All data are expressed as mean±SD. Normality of the data was verified by the Shapiro-Wilk test and all data were normally distributed (p>0.05). Group differences in baseline subject characteristics were analysed using an independent t-test. Two-way repeated ANOVA was conducted on all dependent variables to compare the differences between groups and times. The paired t-test were used to analyse the change values of vascular function within groups (differences between baseline and post-the intervention). Alpha was set at p<0.05. All statistical analyses were performed using SPSS (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp).
Results
Of the twenty participants, two participants in the walking exercise group were unable to complete the entire program due to work circumstances and skin tumor removing surgery, respectively. For the remaining eighteen participants, the adherence to 2 weeks of intervention was 100%. There were no reported changes of exercise according to the health questionnaire. At baseline, no group differences in subject characteristics were found for any variable (Table 1). Following short-term exercise training, there were no significant interaction effects for all dependent variables. As a result of paired t-test, body weight, percent body fat, brachial BP, CDBP, and VO2peakdid not change in any group (p > 0.05, Table 2). However, CSBP decreased in the walking exercise group (97.5 ± 8.8 to 93.6 ± 7.6 mmHg, p < 0.01), but not in the stair climbing exercise group (95.8 ± 6.5 to 93.2 ± 8.3 mmHg, p = 0.135) following exercise training. Also, Changes in c-f PWV was found in stair climbing exercise group (6.83 ± 0.80 to 6.40 ± 0.88 m/s, p = 0.027), but not in the walking exercise group. For percent FMD, both groups exhibited similar improvement following exercise training (stair climbing: 11.49 ± 2.19 to 14.31 ± 2.35%, p = 0.003; walking: 10.83 ± 1.28 to 12.09 ± 2.90%, p = 0.001).
Table 1.
Subject Characteristics
| Stair-Climbing (n=10) |
Walking (n=8) |
p Values |
|
|---|---|---|---|
| Male/Female (n) | 5/5 | 4/4 | |
| Age (yrs) | 21.1±2.3 | 20.8±1.9 | 0.631 |
| Height (cm) | 169.2±9.3 | 166.5±11.4 | 0.277 |
| Weight (kg) | 61.3±11.0 | 59.6±10.1 | 0.575 |
| BMI (kg/m²) | 21.3±2.3 | 21.4±1.8 | 0.865 |
| SBP (mmHg) | 115.4±12.0 | 116.6±13.8 | 0.722 |
| DBP (mmHg) | 69.6±7.6 | 71.1±5.3 | 0.448 |
| CSBP (mmHg) | 95.8±6.5 | 97.5±8.8 | 0.165 |
| CDBP (mmHg) | 67.5±5.1 | 68.1±4.7 | 0.510 |
| c-f PWV (m/s) | 6.83±0.80 | 6.62±0.80 | 0.888 |
| VO2peak (mL/kg/min) | 35.47±7.83 | 37.46±5.21 | 0.151 |
| FMD (%) | 10.62±2.47 | 9.91±1.90 | 0.438 |
| Baseline diameter (mm) | 3.62±0.556 | 3.41±0.393 | 0.390 |
| Max diameter (mm) | 4.03±.0.618 | 3.79±0.468 | 0.363 |
Figure 1.
Individual and mean percentage changes in flow-mediated dilation, and VO2peak after 2 weeks of exercise training
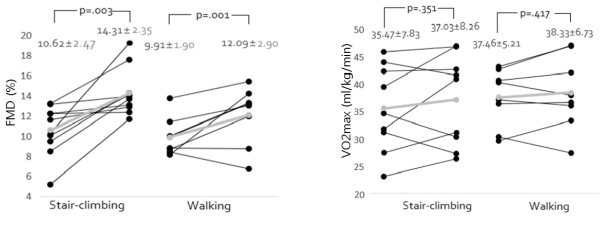
Table 2.
Comparisons of the effects of 2 weeks of stair climbing and walking exercise training
| Stair-Climbing | Walking | p value (group × time) |
|||
|---|---|---|---|---|---|
| Baseline | Post | Baseline | Post | ||
| Weight (kg) | 62.84±11.7 | 62.54±11.7 | 59.55±10.2 | 59.46±10.2 | 0.426 |
| Body fat (%) | 21.66±6.2 | 21.06±6.6 | 22.11±8.0 | 21.9±8.0 | 0.377 |
| HR (bpm) | 62.2±4.8 | 66.6±8.4 | 67.38±5.7 | 67.25±8.7 | 0.333 |
| SBP (mmHg) | 113.2±9.6 | 110.9±11.8 | 114.13±12.8 | 110.25±10.2 | 0.560 |
| DBP (mmHg) | 66.5±5.6 | 64.9±5.8 | 68.25±5.9 | 67.25±4.7 | 0.813 |
| CSBP (mmHg) | 95.8±6.5 | 93.2±8.3 | 97.5±8.8 | 93.6±7.6 ** | 0.541 |
| CDBP (mmHg) | 67.55±5.4 | 65.35±6.0 | 68.06±5.0 | 67.88±4.7 | 0.310 |
| c-f PWV (m/s) | 6.83±0.80 | 6.40±0.88 * | 6.62±0.80 | 6.46±0.85 | 0.356 |
| VO2peak(mL/kg/min) | 35.47±7.83 | 37.03±8.26 | 37.46±5.21 | 38.33±6.73 | 0.726 |
| FMD (%) | 10.62±2.47 | 14.31±2.35 ** | 9.91±1.90 | 12.09±2.90 ** | 0.254 |
| Baseline diameter (mm) | 3.62±0.556 | 3.70±0.598 | 3.41±0.393 | 3.46±0.400 | 0.777 |
| Max diameter (mm) | 4.03±0.618 | 4.23±0.683 | 3.79±0.468 | 3.88±0.529 | 0.540 |
Discussion
The major finding in the present study was that both short-term stair climbing and treadmill walking exercises were comparatively effective in improving arterial stiffness and endothelial function. Our findings suggest that stair climbing exercise may serve as an alternative exercise modality to improve vascular function, especially in worksites and public settings.
Stair climbing exercise can be classified as moderate-to-vigorous intensity physical activity, and the metabolic demand of walking upstairs has been equated to that of running exercise performed at approximately 9.6 km/hour (Ainsworth et al., 2000). In addition, stair climbing can overcome even the most common barriers to exercise, such as lack of time, accessible facilities, special gear, and skills. The effects of stair climbing on aerobic capacity and cardiovascular disease risk factors have been reported in many previous studies. Meyer et al. (2010) has demonstrated that 12 weeks of campaign promoting stair climbing instead of elevator usage were effective in decreasing waist circumference, body fat mass, diastolic BP, and low-density lipoprotein and increasing estimated VO2max by 5.9% in healthy adults. Similarly Boreham et al. (2005) reported a 17.1% increase in VO2peak and a 7.7% decrease in low-density lipoprotein cholesterol in sedentary young healthy women after 8 weeks of stair climbing training, progressively increasing from one ascent a day in first week to five ascents a day in weeks 7 and 8. However, in the present study, there were no changes in body weight, blood pressure and VO2max in both exercise training. The difference in subjects’ characteristics could affect different results from previous studies. There were gender differences in subjects. In Boreham et al. (2005), stair climbing training increased VO2peak in healthy young women. Although the present study was conducted on young men and women, another study (Meyer et al., 2010) reported increase of VO2max and weight loss in both genders. In this regard, the inconsistency between our findings and those of previous studies is likely due to be differences in the duration of exercise training rather than the subjects’ characteristics. In previous studies, weight loss is generally apparent following the long-term (≥8 weeks) exercise training, making it difficult to understand exercise effects independent of weight loss. In our study, the shorter duration of exercise training (2 weeks) did not produce any weight loss and therefore might have contributed to different results compared with those of previous studies. It is important to note that short-term exercise training has been shown to improve arterial stiffness and glucose tolerance without weight loss (Baykara et al., 2017; Cononie et al., 1994). As such, short-term exercise training studies are useful to investigate the effects of exercise itself. In that respect, it is the first study to compare the cardiovascular benefits of short-term stair climbing exercise to regular walking exercise. Considering the effects of stair climbing were similar with traditional aerobic exercise (walking) in this study and the results of previous studies showed the positive changes after stair climbing training, stair climbing exercise can be used as substitute of regular moderate aerobic exercise.
In addition, previous stair climbing studies have focused on improvements in aerobic exercise capacity and traditional cardiovascular risk factors, but information on the effect of stair climbing on vascular health remains unclear. Increased arterial stiffness is an independent predictor of incident CVD and all-cause mortality (Boutouyrie et al., 2002; Vlachopoulos et al., 2010; Laurent et al., 2001). To date, the gold standard measure of arterial stiffness is the measurement of c-f PWV (Laurent et al., 2006), which has been associated vascular damage and incident CVD with increased c-f PWV (Sutton-Tyrrell et al., 2005). Importantly, every 1 m/s increase of PWV has been reported to increase the risk of cardiovascular event and CVD mortality approximately by 12-14% and 13-15%, respectively (Vlachopoulos et al., 2010; Vlachopoulos et al., 2012). Conversely, a 0.63m/s reduction in PWV may translate to an 8% reduction in cardiovascular events and a 9% reduction in cardiovascular mortality (Ashor et al., 2014). Likewise, endothelial dysfunction is an important early stage that precedes the development of atherosclerosis (Deanfield et al., 2007; Ross, 1993) and can be measured via brachial FMD (Yeboah et al., 2009). Importantly, a previous study reported that 1% decrease in brachial FMD is associated with an 8% increase in risk of cardiovascular events (Inaba et al., 2010). Otherwise, a 1% increase in brachial FMD may confer up to a 13% reduction in the risk of incident cardiovascular events (Inaba et al., 2010).
It is well known that regular aerobic exercise is one of the strategies to reduce arterial stiffness and improve endothelial function (Seal et al., 2008; Walther et al., 2004). Consistent with prior studies, we found that while in walking group only FMD increased (2.18%), c-fPWV was significantly decreased (0.43 m/s) and FMD was significantly increased (3.69%) in stair climbing group after 2-week short-term training. Although small, these improvements improvement in vascular function may translate into clinically meaningful changes in terms of risks of cardiovascular events or mortality. Moreover, it is interesting to note that short-term stair climbing exercise can improve vascular function even without apparent changes in VO2peak. Earlier, Green et al. (2014) reported the improvement in endothelial function after training is independent of change in VO2peak. Thus, findings from our study provide new insights regarding the potential benefits of stair climbing exercise on vascular function independent of improvement in risk factors.
The precise mechanisms underlying the benefits of stair climbing exercise on vascular function remain unclear. Generally, aerobic exercise including walking is known to improve endothelial function by increasing blood flow and shear stress on endothelial cells. Likewise, it is possible that stair climbing exercise may induce shear stress on endothelial cells through an increase in blood flow, which subsequently improves their function by increasing the activity of endothelial nitric oxide synthase (eNOS). As a consequence, there can be a structural and functional changes at artery (Jungersten et al., 1997). Moreover, although exercise can increase oxidative stress, exercise-induced oxidative stress improve NO bioavailability (Meilhac et al., 2001). In addition, Pedersen and Febbraio (2012) showed skeletal muscle contraction following stair climbing exercise may stimulate the release of anti-inflammatory cytokines (i.e. interleukin-6), which may further provide positive effects on endothelial function. Future research is warranted to determine the mechanism of stair climbing exercise on vascular function.
There are some limitations of this study. This study was conducted in a small number of healthy young adults. Therefore, the results cannot be generalized to clinical patients or older individuals. In addition, we did not examine directly parameters of oxidative stress or shear rate in this study. Our training duration was only 2 weeks, so the long-term benefits of stair climbing exercise remain to be explored in future studies. Despite of these limitations, this study might have strengths in that it was designed stair climbing as a regular continuous exercise modality, and examined the effects of stair climbing compared with typical aerobic exercise, walking.
In conclusion, short-term stair climbing has similar effect on vascular function with walking exercise in healthy young adults. This might offer new perspective of stair climbing as an exercise modality which is easy to access and perform. Future studies are warranted to explore the physiological mechanisms underlying stair-climbing-induced improvement of vascular function in various subjects.