A 20-year Report on Physical Activity and Obesity among Preschool Children in Western Countries and China
Article information
Abstract
Childhood obesity is a global public health issue. Physical activity (PA) plays an important role in the prevention of becoming obese and reducing the risk of obesity. This study aims to explore the trends of PA and its effects on obesity among preschool children (aged 3–7 years) in different cultural contexts (i.e., Western countries and China). Five databases (English database [PubMed] and four Chinese journal databases [CBM, CNKI, CQVIP, and Wanfangdata]) were searched for studies published between 2002 and 2022. Five Chinese studies were included in the article. These studies demonstrated that comprehensive intervention including PA can prevent and alleviate obesity in preschool children. Eleven English studies met the inclusion criteria, of which seven indicated that the intervention groups reduce obesity among preschool children, while four showed no significant difference. The findings suggest that PA has a discernible impact on obesity in preschool children, highlighting the need for future studies to focus on this specific population to prevent their health better.
Introduction
Obesity is a chronic disease and a risk factor for other conditions such as diabetes, cardiovascular disease, hypertension, and specific types of cancer (Belanger et al., 2016; Nimptsch & Pischon, 2015). Due to the widespread and rapid growth of obesity worldwide and its health risks, it has become a recognized global public health problem. Childhood obesity should be a public health priority because it increases the risk of chronic diseases in adulthood. Compared to children with healthy weights, for example, children under six who are obese are four to five times more likely to become obese once adults (Nimptsch et al., 2019).
Since the 1970s, with the rapid growth of the global economy, obesity among preschool children has become prevalent mainly in developed western countries such as Europe and the USA (Wang & Lobstein, 2006). According to data from the International Obesity Task Force (IOTF) and the WHO, however, childhood obesity rates have increased globally and are no longer a problem only in such developed countries (Low et al., 2009). With continuing economic developments of large countries such as China and India, these numbers are likely to further increase within the next decade (Asia Pacific Cohort Studies Collaboration, 2007). China, as the largest low- and middle-income country, faces a challenge from the burden of obesity. We compared PA and obesity between the Western countries and China to determine if there are differences in the types, intensity, and duration of PA and the relationship of obesity.
For example, the prevalence of obesity has doubled in more than 70 countries since 1980 (Elagizi et al., 2020; The GBD 2015 Obesity Collaborators, 2017). According to the Global Burden of Disease Study, a total of 107.7 million (5%) children worldwide were estimated to be obese in 2015 (GBD 2015 Risk Factors Collaborators, 2016). Moreover, overweight and obesity prevalence taken together was even as high as 23% (GBD 2015 Risk Factors Collaborators, 2016; Ng, 2014).
Obesity is characterized by excess body fat resulting from a positive energy balance (i.e., energy intake greater than energy expenditure) (Dishman et al., 2022). Along with excessive sedentary behavior, calories intake, and poor sleep, lack of PA causes childhood obesity (Hills et al., 2010). The preschool period is debatably considered as a critical period during which the long-term regulation of energy balance may be programmed (Dietz, 1997; Reilly, 2008). In addition to playing a vital role in preventing overweight and obesity, PA is essential for the normal growth and development of children and adolescents (Hills, King, et al., 2007; Hills, Okely, et al., 2010), and reduces the health risks of chronic conditions (Strong et al., 2005).
Most studies on the relationship between obesity and PA focused on adults and adolescents, whereas relevant studies on preschool children remain limited. In China, with the rapid changes in dietary patterns and lifestyles, the problem of childhood obesity has become increasingly serious (Zhang & Ma, 2018).
In this context, the objectives of the report were: 1) to explore the trend of PA and obesity among preschool children in different sociocultural and environment contexts (i.e., western countries and China), and 2) to determine the potential link between PA and obesity in this specific population.
Methods
Search Strategy
We conducted a scoping search on literature written in Chinese and English.
To be completely immerse in the Chinese specific context we chose to search only the Chinese written literature on the topic of PA, obesity, and preschool children. Thus, we searched four of the main Chinese medical databases, including CBM (http://www.sinomed.ac.cn/index.jsp), CNKI (https://www.cnki.net/), CQVIP (http://www.cqvip.com), and Wanfangdata (http://www.wanfangdata.com.cn)] and an English database (PubMed). The period of the literature search was 20 years (from 2002 to 2022). For the Chinese literature search, we used the keywords “肥胖 (obesity)” AND “体育运动 (physical activity)” AND “学龄前儿童 (preschool children)”.
For the English literature search, we used the keywords “obesity” AND “physical activity” AND “preschool children” and focused only on randomized controlled trials (RCTs). We focused on RCTs to ensure the highest evidence level for the cause-and-effect associations between PA and obesity in preschool children.
We finally screened the titles and abstracts of all references for potential correlates of obesity, physical activity, and preschool children to come to the first selection of articles. During a second screening, the remaining papers were fully read to come to the final selection, and after careful consideration, these papers were included in the report.
Inclusion and Exclusion Criteria
The screening was based on inclusion and exclusion criteria.
Inclusion criteria were as follows: (i) studies that examined obesity, (ii) studies that examined correlates of physical activity, (iii) studies with an age range of preschool children from 3 to 7 years old, and (iv) only full-text articles written in Chinese or English. Furthermore, the following exclusion criteria were applied: (i) reviews, (ii) studies that were not conducted on humans, (iii) studies addressing other behaviors (i.e., breastfeeding, nutrition, and diseases), and (iv) studies addressing clinical populations.
Data Extraction and Analysis
We performed data extraction from included studies using a structured form including author, year of publication, country of the study, study sample, follow-up period, target population, obesity prevalence, types of intervention of PA (i.e., questionnaire, accelerometers), and main results.
Results
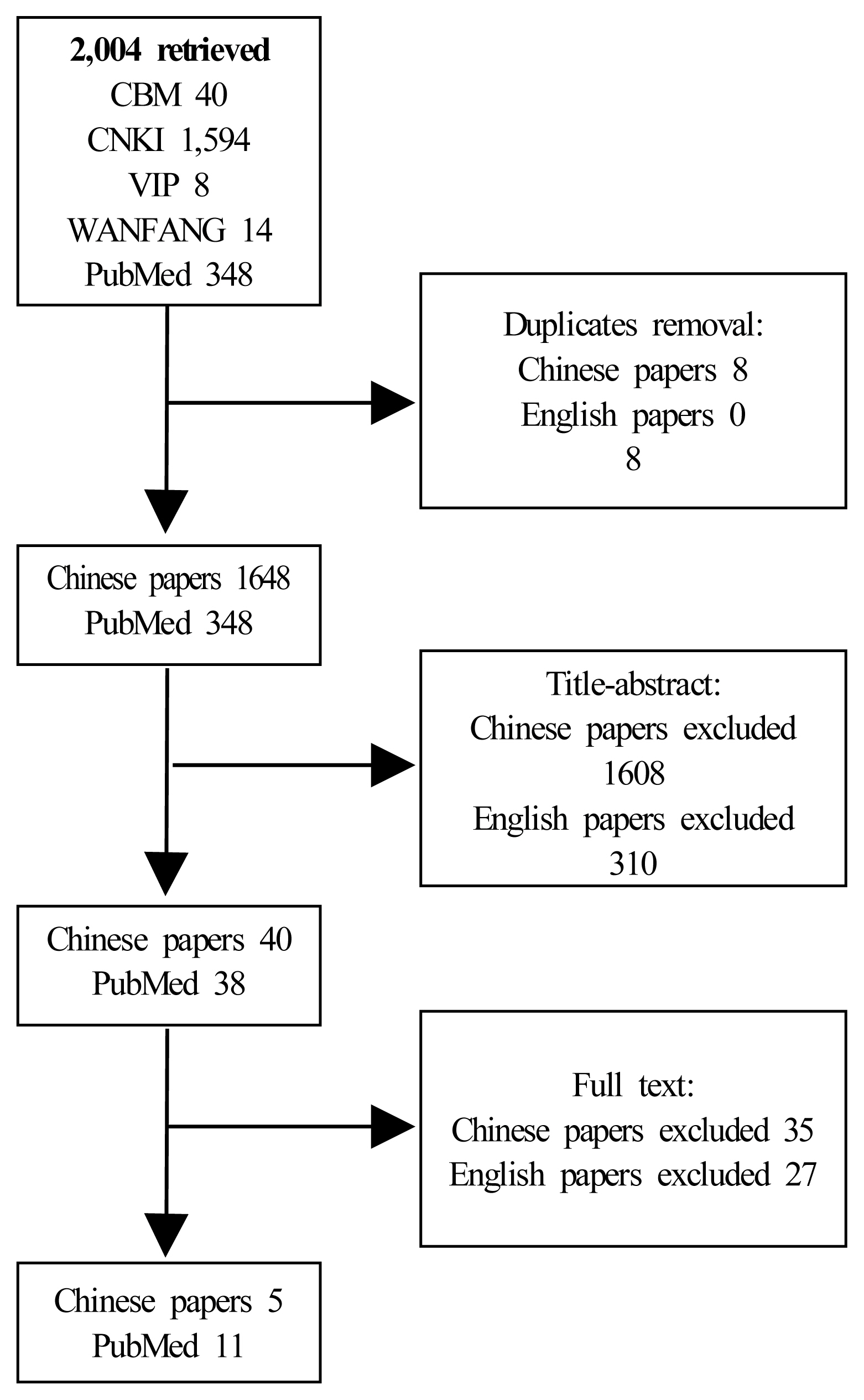
In total, 1,656 Chinese written papers were retrieved (40 in CBM, 1,594 in CNKI, 8 in CQVIP, and 14 in Wanfangdata). After the selection process, five articles were considered in the writing of the report.
In addition, 348 English written RCTs were identified after further selection based on the titles and abstracts and, subsequently, the full text articles. Eleven English published papers were included in the present report. The procedure for excluding papers is reported in Figure 1.
Study Characteristics
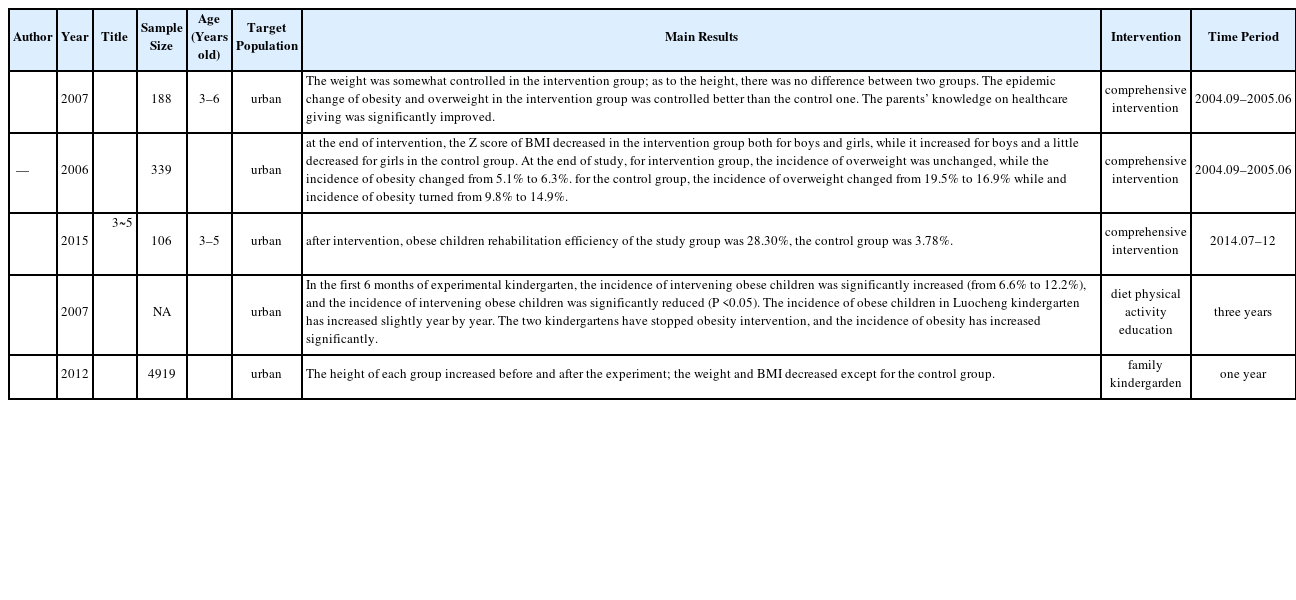
Five published Chinese studies were included in this report. These studies all focused on urban areas. The sample sizes of three studies were between 100 and 999 participants (Jiang et al., 2006; Kong, 2015; Ma et al., 2007). One study enrolled 4919 participants (Xue, 2007). One study included two kindergartens but no specific numbers (Ma et al., 2012). The sample size varied from 106 to 4919 participants.
A total of eleven published English studies were selected. Four were conducted in the USA (Alkon et al., 2014; Annesi et al., 2013; Davis et al., 2016; Kuhl et al., 2014), two of them were conducted in Spain (Llargues et al., 2011; Martinez-Vizcaíno et al., 2020), and the others were conducted in Israel (Eliakim et al., 2007), England (Er et al., 2018), Canada (Goldfield et al., 2016), Scotland (Reilly et al., 2006), and China (Tan et al., 2017). Of the eleven studies included, three studies (27.27%) (Goldfield et al., 2016; Kuhl et al., 2014) had a sample size below 100, six studies (54.54%) (Alkon et al., 2014; Annesi et al., 2013; Er et al., 2018; Llargues et al., 2011; Reilly et al., 2006; Tan et al., 2017) were between 100 and 999, and two studies (18.18%) (Davis et al., 2016; Martinez-Vizcaíno et al., 2020) was above 1000 participants. The sample size varied from 54 to 1898 participants.
Relationship between Physical Activity and Obesity among Preschool Children
In the five Chinese studies, the studies used comprehensive interventions, notably including diet, PA, education, family, and kindergarten. These studies did not explain the relationship between each factor and obesity, and they did not explicitly describe the measurement of PA. These papers showed that the PA measurement was done by recording.
The Table 1 presents Chinese studies’ outcomes, number of participants, follow-up period, target populations, types of interventions, and main results. From table 1, it can be identified that the preschool children were living in urban areas only. The main results are that preschool children’s obesity had been globally reduced through comprehensive intervention.
However, there are some limitations in these Chinese studies. First, these papers did not elaborate on the relationships between diet, PA, education, family, kindergarten and obesity or BMI. Second, the authors generalized the diet, PA, education, family, kindergarten and obesity or BMI, into a whole that they called comprehensive intervention. Therefore, it is difficult to precisely determine why these comprehensive interventions allowed the reduction of preschool children’s obesity. Third, the literature did not describe the types and measurements of PA, or through one sentence detail the types and just recording PA.
For English studies, the interventions were usually precise such as diet or nutrition and PA. The relationship between the intervention factors and preschool children’s obesity was clearly explained. More objective measurements of PA in preschool children (7 studies on 11) were used in these studies such as accelerometers, pedometers, and hand-grip dynamometers. One study used questionnaires, one study recorded the PA, and another two studies did not explain how they measured PA in preschool children.
Seven studies indicated that there were significant differences between intervention groups and control groups. The PA prevented or reduced preschool children’s obesity. However, four studies showed that PA had little effect on obesity at the same time. Six studies of them referred to diet or nutrition and PA. They elaborated on the relationship between diet or nutrition, PA, and obesity separately.
The Table 2 presents English studies’ data outcomes, number of participants, follow-up period, target populations, types of interventions, and main results. The table 2 shows that the target population of the research partly were low-income families living in rural and urban areas. Most of the papers did not precise it. Globally, the main results of these English studies are that children from the intervention group improved their body composition, and increased the time as being physical active.
However, these studies have some limitations. First, using equipment to measure PA may be more objective than questionnaires and recordings, but preschool children are a particular group. They may need to be used to wearing such equipment and taking it off, which may lead to biased results. At the same time, this could require supervision by teachers and parents. Second, although the intervention lasted several weeks, several months, a year or two years, outcomes were assessed immediately after the intervention ended. Thus, there is no data on a long-term effect of such interventions (e.g., measurement 6 months or 1 year after the intervention) in preschool children.
Differences between English Studies and Chinese Studies
Chinese studies recorded PA and did not elaborate on the relationship between PA and obesity. They considered PA, diet, education and other factors as a whole factor, called comprehensive intervention. For researchers, it is difficult to explain the relationships between obesity and one of the Chinese comprehensive interventions.
Most English studies used equipment such as accelerometers or pedometers to record PA, and few studies used questionnaires or recorded PA. Most English research explains the relationships between PA and obesity and brought a more comprehensive explanation of the impacts of PA in very young children.
Discussion
In this present report, five Chinese studies and eleven English studies investigated the link between PA and obesity in preschool children. In the five Chinese studies, the main results indicated that obesity rates have been reduced significantly after the comprehensive interventions including diet, PA and education. In one of these papers (Xue, 2007), the authors divided the population into kindergarten and family interventions. They compared the effect of diet, PA and education separately according to the living areas of the population. Globally they reported that intervention groups presented a decrease in body weight and BMI compared to the control groups.
The five Chinese papers showed that the comprehensive intervention method aimed at dietary adjustment, increasing PA and health education globally prevent obesity prevalence in preschool children. However, it is not possible to precisely determine which factor is essential to obtain such result and no data are available on the effect of the living area on the practice of PA and the prevalence of obesity in these very young children.
In the eleven English articles, Abbey Alkon (Alkon et al., 2014) and Alon Eliakim (Eliakim et al., 2007) agreed that nutrition and PA intervention play a role in health promotion, prevention and treatment of childhood obesity. More precisely, they reported that nutrition and PA intervention can lower BMI for children. Sally M. Davis et al. (2016) believed that at the end of the intervention of eating and exercise, there was no significant difference between the two groups in BMI z-scores. Vanessa Er et al. (2018) found a positive association between PA and BMI z-scores. Likewise, they found evidence of higher PA levels increasing the likelihood of being obese or overweight. Gary S. Goldfifield (2016) and James J. Annesi (2013) reported that increasing PA can significantly reduce children’s BMI. E. S. Kuhl et al. (2014) found that lifestyle behavior including healthy diet, increasing PA and decreasing television time, could help preschoolers achieve healthy weight outcomes. Esteve Llargues et al. (2011) thought that the promotion of healthy eating habits and PA could reduce the prevalence of overweight and obese children. John J Reilly et al. (2006) found that PA can significantly improve motor skills but could not reduce BMI in young children in their trial. Sijie Tan et al. (2017) demonstrated that PA decrease BMI, waist circumference and blood pressure of obese children. Vicente Martínez-Vizcaíno et al. (2020) found no significant improvement in obesity with the intervention compared with the control group. Further, PA did not alter other adiposity indicators and blood pressure parameters in their preschool children.
To sum up, in these English papers, six articles (Alkon et al., 2014; Annesi et al., 2013; Eliakim et al., 2007; Goldfield et al., 2016; Llargues et al., 2011; Tan et al., 2017) showed significant differences between PA and obesity or BMI, meaning that increasing PA effectively reduced BMI or prevented obesity in preschool children. Three articles (Davis et al., 2016; Martinez-Vizcaíno et al., 2020; Reilly et al., 2006) indicated that after interventions of PA, there was no significant difference between the intervention and the control group concerning the BMI. One article (Er et al., 2018) showed that higher PA levels increased the likelihood of being obese and one paper (Kuhl et al., 2014) showed that preschoolers experienced a significant decrease in BMI after the lifestyle behaviors changes (e.g., reduction of sugar-sweetened beverage intake, increased fruit and vegetable intake, increased PA, and decreased television time).
The included Chinese studies and English studies show that obesity is relieved through comprehensive intervention or PA. However, most English studies tried to explain and describe the relationships between PA and obesity, or BMI and Chinese studies did not. They usually use comprehensive factors like diet, PA, family, kindergarten together to describe preschool children’s obesity and trend of PA.
Overall, for the majority of English studies and for all Chinese studies included in the present report, results implied that PA is helpful for the prevention of obesity in preschool children. The PA can improve obesity among preschool children. It is noteworthy that three English studies indicated no statistically significant relationship between PA and obesity and one study showed that increased PA increase the likelihood of being obese. These discrepancies are commonly due to the lack of objective measures of PA. Thus, it is not clear whether social and cultural environment could influence obesity and the practice of PA in preschool children. In addition, it is not possible to determine what kind of PA is useful to prevent obesity in preschool children and what are the physiological effects behind this prevention.
According to the World Health Organization (WHO) recommendations, the PA protects children against the occurrence of overweight and obesity (Baran et al., 2020). Research studies have shown that preschool children do not regularly engage in the recommended 60 minutes of moderate to vigorous PA each day (Wolfenden et al., 2011), while other studies found that they spend much of their time in sedentary behaviors (Pate et al., 2008; Reilly, 2010). One study found that children spend more time in moderate to vigorous physical activity when childcare programs have moveable playground equipment (e.g., balls, tricycles), lower use of electronic media, and larger playgrounds compared to programs without these characteristics (Dowda et al., 2009).
Based on the above discussions, we suggest that preschool children should do moderate PA, not only to keep from becoming obese during their adulthood, but also for their health and growth.
To the extent of our knowledge, it is the first report describing trends in PA and obesity among preschool children in Western countries and China. Despite the tendency of a global beneficial effect of PA on obesity in preschool children in Western countries and China they are some issues concerning the type of PA, the intensity, the duration, the frequency of PA, the objective measurement of PA and its real physiological and cognitive impacts on these very young children. There are also issues concerning the differential impact of PA between very young girls and boys. In this context, we suggest that preschool children may benefit from small sessions of PA (30 minutes per day), every days of the week using the high intensity interval training type (high intensity PA sessions interspaced by period of rest). PA should focus on all part of the children’s body (lower and upper limbs) to expect a global effect for the development of their bones and muscles. PA sessions should include game and group interactions which may increase the motivation of children to exercise. In the absence of clear preschool children PA recommendations, we hypothesize that this kind of PA should be effective to prevent obesity in preschool children.
Limitations
The present report has some limitations. First, is was difficult to find Chinese papers in Chinese scientific database depending of the sonogram used and its multiple signification. That is why we precised the sonograms used in this report. In addition, Miss Jianhong Han is Chinese so it helps a lot for this part of the search. Second, it was difficult to compare western countries and China results because of the small number of papers concerned. However, this put in evidence the need of research in this important topic to prevent obesity in very young children all other the world. Finally, the present report was not registered in PROSPERO but this is not a systematic review or a meta-analysis. We used the word “report” rather than “review” for this reason. However, this not preclude the quality and integrity of the contents in the present report.
Conclusion
The aim of the current report was to explore the trends and effects of PA on obesity among preschool children in different sociocultural and environment contexts (western countries and China).
Of the included five Chinese studies and eleven English studies, twelve papers of them demonstrated that PA improved the situation of obesity in preschool children, except four English studies. All Chinese studies and most of the English studies conclude that PA reduces obesity to a certain extent. However, some English studies show no statistically significant relationship between PA and obesity and one study showed that increased PA increases the likelihood of being obese. Based on these findings, it can be inferred that adequate PA may prevent preschool children’s obesity and is beneficial for the health and growth of preschool children. Future studies are needed to precise the types of PA, its intensity, frequency, duration and to explore the social and cultural impacts on the active behavior of preschool children and the prevalence of obesity in this specific population. FAt the same time, future research is needed to explore what types of PA and PA intensity are more effective for preventing obesity in preschool children.
Acknowledgments
This research was financially supported by China Scholarship Council.
Notes
Authors’ Contributions
Damien Vitiello conceived the study, participated in its disign and coordination and helped to revise the manuscript; Jianhong Han performed the data collection/sorting and drafted the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing Interests
The authors declare that they have no competing interests.