 |
 |
| Int J Appl Sports Sci > Volume 34(2); 2022 > Article |
|
Abstract
Lateral ankle sprain (LAS) is the most common injury in youth soccer. The mechanisms of LAS should be identified to develop effective injury prevention programs. Alignment and range of motion (ROM) are considered factors affecting kinematics during movement. Therefore, this study was designed to identify whether static measurements, including alignment and ROM, affect ankle kinematics related to LAS during running in youth soccer players. For this study, 100 participants were recruited. Data on rearfoot angle in the prone position (PRA), tibial varum, weight-bearing lunge test (WBLT), passive eversion, passive inversion (PIN), and ankle kinematics during running of all participants were collected. Ankle kinematics were computed for dorsiflexion at the initial contact (IC), inversion at IC, maximum dorsiflexion (MDF), and maximum inversion (MIN). Stepwise multiple regressions were conducted with an alpha level of 0.05. PRA, WBLT, and PIN significantly predicted dorsiflexion at IC (R2 = 0.144, P < 0.001), and PRA was a significant predictor on inversion at IC (R2 = 0.227, P < 0.001). PRA and WBLT were significant predictors on MDF (R2 = 0.330, P < 0.001), and PRA significantly predicted MIN (R2 = 0.188, P < 0.001). Of significant predictors, only WBLT can be treated by joint mobilization. Thus, WBLT related to pronation, which makes the ankle in a closed-packed position, should be treated to increase DF ROM and ankle stability. In addition, low-speed running video analysis might be useful in screening for ankle malalignment.
Lateral ankle sprain (LAS) is one of the most common injuries among soccer players (Emery et al., 2005; Giza & Micheli, 2005; Kucera et al., 2005; Le Gall et al., 2006). A LAS tends to cause musculoskeletal problems, such as chronic ankle instability (CAI) (Gribble et al., 2014; Hertel, 2000), ankle osteoarthritis (Gross & Marti, 1999; Harrington, 1979), altered biomechanics (Drewes et al., 2009a; Drewes et al., 2009b), and decreased physical activity (Hubbard-Turner & Turner, 2015), patient-oriented outcomes (Choi & Shin, 2015; Lee et al., 2021), and health-related quality of life (HR-QoL) (Gigi et al., 2015; Lee et al., 2021; Simon & Docherty, 2018). Moreover, a systematic review of prospective epidemiological studies of LAS has reported that the affected population is getting younger and the incidence of LAS is increasing (Doherty et al., 2014). Additionally, adolescent athletes experience growth spurts, which may make them vulnerable to injury by causing increased tension in soft tissues, such as ligaments and tendons (Micheli & Klein, 1991). In Korean youth soccer, the ankle joint and ligament sprain were reported as the most common body location and type of injury, respectively (Lee et al., 2020b). Given the aforementioned comprehensive problems, injuries during adolescence may have negative effects on physical growth, performance enhancement, careers, and HR-QoL. Therefore, preventing injury is crucial in youth soccer players.
Finch (2006) has suggested using the Translating Research into Injury Prevention Practice (TRIPP) model to develop evidence-based injury prevention programs. In the TRIPP model, epidemiological studies and establishment of mechanisms of injury (MOIs) should precede the development of preventive programs. Epidemiological studies for LAS in Korean youth soccer players were conducted (Lee et al., 2020a). The study identified that a total of 76 LAS were reported from 69 of 681 players for a season (Lee et al., 2020a). In addition, the most cause of LAS was non-contact injury and days to full training were 20 days with 36.84% of reinjury rate (Lee et al., 2020a). Therefore, MOIs should be established to develop evidence-based injury prevention programs for preventing LAS in Korean youth soccer. The International Ankle Consortium has suggested that clinical factors should be assessed following an acute LAS (Delahunt et al., 2018), indicating that those factors are affected by LAS. Of those factors mentioned in the previous study (Delahunt et al., 2018), gait should be assessed because altered gait biomechanics were observed in previous studies (Brown et al., 2008; Delahunt et al., 2006; Doherty et al., 2016; Drewes et al., 2009a; Drewes et al., 2009b; Lee et al., 2022; Monaghan et al., 2006).
Previous studies reported dorsiflexion deficits and more inverted ankle in individuals with CAI during gait consistently (Brown et al., 2008; Delahunt et al., 2006; Doherty et al., 2016; Drewes et al., 2009a; Drewes et al., 2009b; Lee et al., 2022; Monaghan et al., 2006). Dorsiflexion is the motion occurring in the sagittal plane while inversion is generated in the frontal plane. Dorsiflexion deficits may have the ankle on the open-packed position of the joint, making the ankle unstable in individuals with ankle dysfunction. Furthermore, more inverted ankles may directly affect the occurrence of LAS during gait by changing ankle kinematics. Inversion (IN) is the main component of MOI of LAS and lengthens the anterior talofibular and calcaneofibular ligaments (Gribble et al., 2014; Hertel, 2002), which may predispose an individual with more inverted ankle to LAS. Given anatomical characteristics, altered ankle kinematics in the sagittal and frontal planes reported in previous studies may cause LAS (Brown et al., 2008; Delahunt et al., 2006; Doherty et al., 2016; Drewes et al., 2009a; Drewes et al., 2009b; Lee et al., 2022; Monaghan et al., 2006). Thus, identifying what factors affect the ankle kinematics during gait, especially running, is needed because running is a basic movement skill in soccer.
Human movement strategies are decided by a combination of body structures and physical function. Body structures, such as alignment work with physical function, including joint range of motion (ROM), strength, endurance, and power. Alignments may decide the joint kinematics for the initial contact (IC) during the swing phase, and joint ROM presents flexibility, which may affect comfortable postures. Given that human movements are based on energy efficiency, alignments and joint ROM may be important factors for movement strategies (Boozer et al., 2002; Kang & Oh, 2017; Lee & Hertel, 2012; McPoil & Cornwall, 1996), indicating that ankle kinematics during running may be affected by alignments and ROM. Therefore, this study was designed to identify significant factors for static measurements affecting ankle kinematics in the sagittal and frontal planes during running in youth soccer players.
A cross-sectional study design was adopted. This study was approved by the Institutional Review Board of Yonsei University (7001988-202011-HR-1045-02), and all participants signed written informed consent voluntarily. We complied with the rules of the 1975 Declaration of Helsinki, revised in 2013. After an explanation on and agreement with this study, the participants’ basic information was collected. Basic information included age, career, dominant leg, height, and weight. Then, static measurements and ankle kinematics during running were performed.
For this study, 106 participants were initially recruited from two Korean U-15 elite soccer teams. We screened the participants based on the following five eligibility criteria. First, the participants should be between 12 and 15 years old. Second, the participants should be registered in the Korea Football Association. Third, the participants should conduct at least three training sessions per week. Fourth, the participants should have no history of musculoskeletal injuries within 3 months before the data collection. Fifth, the participants should be able to perform clinical tests without any problem. After screening, six participants were excluded because of recent injury histories. Therefore, a total of 100 youth soccer players participated in this study. The demographic characteristics of all participants are shown in Table 1.
All data collection was conducted by investigators with good and excellent intra-rater reliability (Table 2). Intra-rater reliability was identified by the intraclass correlation coefficient (ICC). ICC was interpreted based on the following criteria (Koo & Li, 2016): poor, ICC < 0.5; moderate, 0.5 ≤ ICC < 0.75; good, 0.75 ≤ ICC < 0.9; excellent, ICC ≥ 0.9.
Static measurements for this study included lower-extremity alignments and ankle ROM. Rearfoot angle in the prone position (PRA) and tibial varum (TV) were collected for alignments, while the weight-bearing lunge test (WBLT) on dorsiflexion (DF) ROM under a weight-bearing condition, passive eversion (PEV), and passive IN (PIN) were measured for ankle ROM. For the PRA measurement, the participants were instructed to lie prone on the bed with the ankle out of the edge of the bed. The investigator identified the subtalar neutral position, palpating the medial and lateral portions of the talar head equally using the thumb and index finger. Then, the angle between two lines—one line was the midline of calcaneus and the other one was the bisecting line of the Achilles tendon—was measured (Buchanan & Davis, 2005). For TV measurement, the participants lay prone similar to that in PRA measurements; the angle between the bisecting lines of the upper two-thirds and lower one-third of the lower leg was measured (Tomaro, 1995). For WBLT (Kang et al., 2015), the participants stood on a straight line with one leg front and the other one back. Then, the participants’ dorsiflexed the ankle of the front leg with the knee front toward the second toe line forward. The investigator measured the angles between the vertical line and tibial shaft using a digital inclinometer (iPhone XS, Apple Inc., Cupertino, CA, US). For PEV and PIN, the participants sat on the bed with the hip and knee joint at 90° flexion. The axis of ROM was defined as the midpoint between the medial and lateral malleoli. The stationary arm was aligned with the bisecting line of the anterior tibia shaft. The moving arm was aligned with the line of the second ray of the food. The investigator made maximum ankle eversion and inversion of the participants and measured the ROM (Menadue et al., 2006).
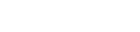
Ankle kinematics during running were analyzed for dependent variables. The experimental setting for ankle kinematics during running is shown in Figure 1. Ankle kinematics during running were analyzed using video analysis. The investigator instructed the participants to run lightly at the preferred speed throughout a 9-m runway thrice. All trials were recorded using three cameras (EOS 5D Mark 2, Canon Inc., Ohta-ku, Tokyo, Japan) with a sampling rate of 30 frame/s. Each one running cycle for three trials was analyzed in the sagittal and frontal planes. The dependent variables on ankle kinematics during running were DF at IC, IN at IC, maximum DF (MDF), and maximum IN (MIN). All joint angles were computed by Kinovea software 0.8.15 (Kinovea open-source project, www.kinovea.org). For the sagittal ankle motion (Fernández-González et al., 2020; Schurr et al., 2017), DF was calculated using the following formula: DF = 90-(the angle between the line from the lateral epicondyle to the lateral malleoli and the line parallel to the 5th metatarsal). For the ankle joint angle in the frontal plane (Fernández-González et al., 2020; Schurr et al., 2017), IN was defined as the angle between two lines: the first line was from the midpoint between the medial and lateral epicondyle to the midpoint between the medial and lateral malleoli and the other one was the bisecting line of the calcaneus. The preferred running speed was calculated using the following formula: the preferred running speed (m/s) = 5 m/the time spent on finishing the 5-m course throughout the video-recording area (s).
Two hundred limbs from 100 participants were analyzed. The mean and standard deviations for all variables were calculated. Independent variables were static measurements, including WBLT, PEV, PIN, PRA, and TV. Dependent variables were ankle kinematics during running, including DF at IC, IN at IC, MDF, and MIN during a gait cycle. Multiple linear regressions with stepwise selection were used to identify factors significantly affecting the ankle kinematics in the sagittal and frontal planes during running in youth soccer players. An alpha level was set at 0.05 for all statistical analyses. All analyses were performed using Statistical Package for the Social Sciences (version 25; IBM Corporation, Armonk, NY, USA).
The multiple linear regressions were used to determine which factors of static measurements significantly predict ankle kinematics during running. Descriptive statistics for all variables are presented in Table 3. The overall models on each multiple linear regression analysis were statistically significant (P < 0.001). For DF at IC, the explanatory power of the regression model was 15.7%, and WBLT, PRA, and PIN were significant independent variables (P = 0.049) (Table 4). The regression equation for DF at IC was as follows: DF at IC = −3.777 + (0.353 × WBLT) + (−0.444 × PRA) + (−0.102 × PIN). The explanatory power of the IN at IC regression model was 23.1%, and PRA was a significant independent variable (P < 0.001) (Table 5). The regression equation for IN at IC was as follows: 0.528 + (0.365 × PRA). For MDF, the explanatory power of the regression model was 33.7%, and WBLT and PRA were significant independent variables (P = 0.001) (Table 6). The regression equation for MDF was as follows: 5.349 + (0.297 × WBLT) + (−0.210 × PRA). The explanatory power of the MIN was 19.2%, and PRA was a significant independent variable (P < 0.001) (Table 7). The regression equation on MIN was as follows: 5.031 + (0.227 × PRA).
This study was conducted to identify whether static measurements significantly affect ankle kinematics during running in youth soccer players to develop evidence-based injury prevention programs. Our findings showed that PRA, WBLT, and PIN were significant predictors of DF at IC, whereas only PRA significantly predicted IN at IC. Furthermore, PRA and WBLT significantly predicted MDF, whereas only PRA was a significant predictor of static measurements on MIN.
The ankle complex consists of the talocrural and subtalar joints, and each joint has their own oblique axis of rotation (Hertel, 2002). The oblique axis is not strictly perpendicular to cardinal planes. Therefore, the rearfoot moves as a unit in triplanar motions but not isolated motions in the individual planes (Hertel, 2002). Triplanar motions of the ankle are divided into supination and pronation. Supination consists of plantar flexion, IN, and adduction, whereas pronation is composed of DF, EV, and abduction. Moreover, supination causes an open-packed position, which decreases joint stability, whereas pronation results in a closed-packed position, which increases the joint surface congruity. Interestingly, the lateral ligaments of the ankle are damaged by LAS with excessive supination (Gribble et al., 2014; Hertel, 2000), indicating that IN is the main component of the LAS MOI in an open-packed position. Individuals with CAI tended to walk with dorsiflexion deficits and more inverted ankles compared to healthy controls (Brown et al., 2008; Delahunt et al., 2006; Doherty et al., 2016; Drewes et al., 2009a; Drewes et al., 2009b; Lee et al., 2022; Monaghan et al., 2006). Therefore, decreased supination and increased pronation should be emphasized to prevent LAS during gait. In this study, PRA, WBLT, and PIN are significant predictors of ankle kinematics, which were consistent with the findings in a previous study (Kang & Oh, 2017). Of the significant predictors in this study, PRA and PIN are related to supination and WBLT is associated with pronation. Because PRA is a variable of lower-extremity alignment and PIN is a variable of passive ROM, those may be unable to be controlled by interventions. However, WBLT is a variable of active ROM using own body weight, which could be treated with joint mobilization. A previous systematic review and meta-analysis identified that joint mobilization has significant effects on DF ROM and dynamic postural control (Vallandingham et al., 2019). Thus, because PRA related to supination could not be treated, clinicians and exercise specialists should focus on increasing pronation using joint mobilization for DF ROM to prevent LAS.
The oblique axes of the ankle complex affect not only the rearfoot but also the lower leg (Pohl et al., 2006). Rearfoot supination is related to tibial external rotation, and pronation is associated with tibial internal rotation. Given the reason, although decreased supination and increased pronation may help prevent LAS, those mechanisms may cause limited function caused by closed-packed position and abnormal stress to musculoskeletal structures in the proximal segment or joint. Excessive pronation of the ankle has been considered a risk factor for various injuries, such as medial tibial stress syndrome (Okunuki et al., 2019), plantar fasciitis (Luffy et al., 2018), high ankle sprain (Bellows & Wong, 2018), and patellar femoral pain syndrome (Boling et al., 2009). Therefore, when preventing LAS and other injuries, controlling pronation should be focused and studied in future studies.
The task conducted in this study may be a relatively low intensity activity because it was running on the straight line at the preferred speed. However, it may indicate that our findings can apply to more complex task than the task conducted in this study. Therefore, the results of this study must not be overlooked, and more studies should be carried out in the future. Furthermore, our findings may indicate that low-speed running video analysis is also useful to identify malalignment of the ankle joint. Because malalignment is related to overuse injuries as well as LAS, it may be effective on movement screening and detecting risk factors in sports fields. However, there is a lack of studies on relationships between static measurements and movement patterns of not only ankle but other joints. Thus, future studies are needed to identify relationships more variables of alignment and ROM and movement patterns.
This study had some limitations. First, only five static measurements were entered into the regression models, which may have limited the explanatory power. Therefore, more variables of static measurements are needed to explain and predict ankle kinematics more accurately. Second, the participants in this study were recruited regardless of the presence or absence of a history of LAS. Thus, future studies should identify LAS-specific associations between static measurements and ankle kinematics by recruiting participants with a LAS history. However, the study strengths were as follows: big sample size, data collection by investigators with good reliability, and the use of readily available clinical methods. Static measurement data collected by an investigator with a high level of intra-rater reliability and a big sample size are essential for accurately predicting ankle kinematics during dynamic tasks (McPoil and Cornwall, 1996). Despite the aforementioned limitations, our findings were valuable and helpful in developing LAS prevention programs for youth soccer players.
PRA, WBLT, and PIN of static measurements were significant predictors of ankle kinematics during running in youth soccer players. Of those, only WBLT can be treated using joint mobilization to increase DF ROM and ankle stability. In addition, low-speed running video analysis conducted in this study might be useful as screening in identify ankle kinematics and malalignment, which may be related to LAS.
Acknowledgment
This work was supported by the Yonsei University Research Grant of 2021. The authors would like to thank all participants for their support and contributions to this study. We also appreciate the International Olympic Committee Research Centre KOREA and the Institute of Convergence Science.
Table 1
Demographic characteristics of participants
| Variable | Value (N = 100) |
|---|---|
| Age (years)a | 13.2 ± 1.0 |
| Height (m)a | 1.62 ± 0.09 |
| Body mass (kg)a | 53.37 ± 9.54 |
| Body mass index (kg/m2)a | 20.06 ± 2.08 |
| Career (year)a | 3.95 ± 1.96 |
| Preferred running speed (m/s)a | 2.68 ± 0.33 |
| Dominant leg (L:R) | 11:89 |
Table 2
Reliability on measurements of investigation
| Category | Variable | ICC(2,1) | 95% CI | P-Value |
|---|---|---|---|---|
| Lower extremity alignment | Prone rearfoot angle | 0.856 | 0.247-0.984 | 0.009** |
| Tibial varum | 0.826 | 0.057-0.987 | 0.030* | |
|
|
||||
| Range of motion | Weight bearing lunge test | 0.974 | 0.739-0.998 | 0.003** |
| Passive eversion | 0.905 | 0.206-0.976 | 0.017* | |
| Passive inversion | 0.874 | 0.471-0.971 | 0.007** | |
|
|
||||
| Ankle kinematics during running using video analysis | Sagittal plane motion | 0.942 | 0.635-0.994 | 0.002** |
| Frontal plane motion | 0.958 | 0.582-0.996 | <0.001*** | |
Table 3
Descriptive statistics of static measurements and ankle kinematics during running
Table 4
Significant predictors of static measurements on dorsiflexion at the initial contact
| Variable | Unadjusted β a | P | Adjusted β a | P |
|---|---|---|---|---|
| Prone rearfoot angle (°) | −0.422 (0.155) | 0.007** | −0.444 (0.146) | 0.003** |
| Tibial varum (°) | 0.347 (0.294) | 0.240 | ||
| Weight-bearing lunge test (°) | 0.342 (0.072) | <0.001*** | 0.353 (0.070) | <0.001*** |
| Passive eversion (°) | −0.021 (0.053) | 0.696 | ||
| Passive inversion (°) | −0.082 (0.055) | 0.137 | −0.102 (0.051) | 0.049* |
|
|
||||
| A model summary of multiple linear regression: R2 = 0.157; adjusted R2 = 0.144; P < 0.001*** | ||||
Table 5
Significant predictors of static measurements on inversion at the initial contact
| Variable | Unadjusted β a | P | Adjusted β a | P |
|---|---|---|---|---|
| Prone rearfoot angle (°) | 0.365 (0.047) | < 0.001*** | 0.365 (0.047) | < 0.001*** |
| Tibial varum (°) | 0.063 (0.101) | 0.537 | ||
| Weight-bearing lunge test (°) | <0.001 (0.026) | 0.988 | ||
| Passive eversion (°) | 0.029 (0.018) | 0.112 | ||
| Passive inversion (°) | 0.012 (0.019) | 0.513 | ||
|
|
||||
| A model summary of multiple linear regression: R2 = 0.231; adjusted R2 = 0.227; P < 0.001*** | ||||
Table 6
Significant predictors of static measurements on maximum dorsiflexion
| Variable | Unadjusted β a | P | Adjusted β a | P |
|---|---|---|---|---|
| Prone rearfoot angle (°) | −0.200 (0.078) | 0.011* | −0.210 (0.065) | 0.001** |
| Tibial varum (°) | 0.141 (0.148) | 0.343 | ||
| Weight-bearing lunge test (°) | 0.296 (0.032) | <0.001*** | 0.297 (0.031) | <0.001*** |
| Passive eversion (°) | −0.001 (0.027) | 0.980 | ||
| Passive inversion (°) | 0.019 (0.028) | 0.499 | ||
|
|
||||
| A model summary of multiple linear regression: R2 = 0.337; adjusted R2 = 0.330; P < 0.001*** | ||||
Table 7
Significant predictors of static measurements on maximum inversion
| Variable | Unadjusted β a | P | Adjusted β a | P |
|---|---|---|---|---|
| Prone rearfoot angle (°) | 0.227 (0.033) | <0.001*** | 0.227 (0.033) | <0.001*** |
| Tibial varum (°) | 0.113 (0.068) | 0.100 | ||
| Weight-bearing lunge test (°) | 0.002 (0.018) | 0.918 | ||
| Passive eversion (°) | 0.017 (0.012) | 0.159 | ||
| Passive inversion (°) | 0.001 (0.013) | 0.914 | ||
|
|
||||
| A model summary of multiple linear regression: R2 = 0.192; adjusted R2 = 0.188; P < 0.001*** | ||||
References
Bellows, R., & Wong, C. K. (2018). The effect of bracing and balance training on ankle sprain incidence among athletes: A systematic review with meta-analysis. International Journal of Sports Physical Therapy, 13(3), 379-388.



Boling, M. C., Padua, D. A., Marshall, S. W., Guskiewicz, K., Pyne, S., & Beutler, A. (2009). A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. The American Journal of Sports Medicine, 37(11), 2108-2116.


Boozer, M. H., Finch, A., & Waite, L. R. (2002). Investigation of the relationship between arch height and maximum pronation angle during running. Biomedical Sciences Instrumentation, 38, 203-207.

Brown, C., Padua, D., Marshall, S. W., & Guskiewicz, K. (2008). Individuals with mechanical ankle instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clinical Biomechanics, 23(6), 822-831.


Buchanan, K. R., & Davis, I. (2005). The relationship between forefoot, midfoot, and rearfoot static alignment in pain-free individuals. Journal of Orthopaedic & Sports Physical Therapy, 35(9), 559-566.


Choi, H.-S., & Shin, W.-S. (2015). Validity of the lower extremity functional movement screen in patients with chronic ankle instability. Journal of Physical Therapy Science, 27(6), 1923-1927.



Delahunt, E., Bleakley, C. M., Bossard, D. S., Caulfield, B. M., Docherty, C. L., Doherty, C., & Hiller, C. E. (2018). Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement & recommendations of the International Ankle Consortium. British Journal of Sports Medicine, 52(20), 1304-1310.

Delahunt, E., Monaghan, K., & Caulfield, B. (2006). Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. The American Journal of Sports Medicine, 34(12), 1970-1976.



Doherty, C., Bleakley, C., Hertel, J., Caulfield, B., Ryan, J., & Delahunt, E. (2016). Locomotive biomechanics in persons with chronic ankle instability and lateral ankle sprain copers. Journal of Science and Medicine in Sport, 19(7), 524-530.


Doherty, C., Delahunt, E., Caulfield, B., Hertel, J., Ryan, J., & Bleakley, C. (2014). The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Medicine, 44(1), 123-140.



Drewes, L. K., McKeon, P. O., Kerrigan, D. C., & Hertel, J. (2009a). Dorsiflexion deficit during jogging with chronic ankle instability. Journal of Science and Medicine in Sport, 12(6), 685-687.


Drewes, L. K., McKeon, P. O., Paolini, G., Riley, P., Kerrigan, D. C., Ingersoll, C. D., & Hertel, J. (2009b). Altered ankle kinematics and shank-rear-foot coupling in those with chronic ankle instability. Journal of Sport Rehabilitation, 18(3), 375-388.


Emery, C. A., Meeuwisse, W. H., & Hartmann, S. E. (2005). Evaluation of risk factors for injury in adolescent soccer: implementation and validation of an injury surveillance system. The American Journal of Sports Medicine, 33(12), 1882-1891.

Fernández-González, P., Koutsou, A., Cuesta-Gómez, A., Carratalá-Tejada, M., Miangolarra-Page, J. C., & Molina-Rueda, F. (2020). Reliability of kinovea® software and agreement with a three-dimensional motion system for gait analysis in healthy subjects. Sensors, 20(11), 3154.


Finch, C. (2006). A new framework for research leading to sports injury prevention. Journal of Science and Medicine in Sport, 9(1-2), 3-9.


Gigi, R., Haim, A., Luger, E., Segal, G., Melamed, E., Beer, Y., & Elbaz, A. (2015). Deviations in gait metrics in patients with chronic ankle instability: A case control study. Journal of Foot and Ankle Research, 8(1), 1-8.




Giza, E., & Micheli, L. J. (2005). Soccer injuries. Epidemiology of Pediatric Sports Injuries, 49, 140-169.

Gribble, P. A., Delahunt, E., Bleakley, C., Caulfield, B., Docherty, C., Fourchet, F., & Kaminski, T. (2014). Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. British Journal of Sports Medicine, 48(13), 1014-1018.


Gross, P., & Marti, B. (1999). Risk of degenerative ankle joint disease in volleyball players: Study of former elite athletes. International Journal of Sports Medicine, 20(1), 58-63.


Harrington, K. (1979). Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. The Journal of Bone and Joint Surgery. American Volume, 61(3), 354-361.


Hertel, J. (2000). Functional instability following lateral ankle sprain. Sports Medicine, 29(5), 361-371.


Hertel, J. (2002). Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. Journal of Athletic Training, 37(4), 364


Hubbard-Turner, T., & Turner, M. J. (2015). Physical activity levels in college students with chronic ankle instability. Journal of Athletic Training, 50(7), 742-747.




Kang, M.-H., Lee, D.-K., Park, K.-H., & Oh, J.-S. (2015). Association of ankle kinematics and performance on the y-balance test with inclinometer measurements on the weight-bearing-lunge test. Journal of Sport Rehabilitation, 24(1), 62-67.


Kang, M.-H., & Oh, J.-S. (2017). Relationship between weightbearing ankle dorsiflexion passive range of motion and ankle kinematics during gait. Journal of the American Podiatric Medical Association, 107(1), 39-45.



Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155-163.



Kucera, K. L., Marshall, S. W., Kirkendall, D. T., Marchak, P., & Garrett, W. E. (2005). Injury history as a risk factor for incident injury in youth soccer. British Journal of Sports Medicine, 39(7), 462-462.



Le Gall, F, Carling, C, Reilly, T, Vandewalle, H, Church, J, & Rochcongar, P (2006). Incidence of injuries in elite French youth soccer players: A 10-season study. The American Journal of Sports Medicine, 34(6), 928-938.

Lee, I., Ha, S., Chae, S., Jeong, H. S., & Lee, S. Y. (2022). Altered biomechanics in individuals with chronic ankle instability compared with copers and controls during gait. Journal of Athletic Training, 57(8), 760-770.



Lee, I., Jeon, H. G., Jeong, H. S., Kang, T. K., & Lee, S. Y. -2020a. An epidemiological study of ankle sprains in youth soccer. Journal of Sport and Leisure Studies, 82, 425-432.

Lee, I., Jeong, H. S., & Lee, S. Y. (2020b). Injury profiles in korean youth soccer. International Journal of Environmental Research and Public Health, 17(14), 5125.



Lee, I., Lee, S. Y., & Ha, S. (2021). Alterations of lower extremity function, health-related quality of life, and spatiotemporal gait parameters among individuals with chronic ankle instability. Physical Therapy in Sport, 51, 22-28.


Lee, S. Y., & Hertel, J. (2012). Arch height and maximum rearfoot eversion during jogging in 2 static neutral positions. Journal of Athletic Training, 47(1), 83-90.




Luffy, L., Grosel, J., Thomas, R., & So, E. (2018). Plantar fasciitis: A review of treatments. Journal of the American Academy of PAs, 31(1), 20-24.
McPoil, T. G., & Cornwall, M. W. (1996). The relationship between static lower extremity measurements and rearfoot motion during walking. Journal of Orthopaedic & Sports Physical Therapy, 24(5), 309-314.


Menadue, C., Raymond, J., Kilbreath, S. L., Refshauge, K.M., & Adams, R. (2006). Reliability of two goniometric methods of measuring active inversion and eversion range of motion at the ankle. BMC Musculoskeletal Disorders, 7(1), 1-8.




Micheli, L. J., & Klein, J. (1991). Sports injuries in children and adolescents. British Journal of Sports Medicine, 25(1), 6-9.



Monaghan, K., Delahunt, E., & Caulfield, B. (2006). Ankle function during gait in patients with chronic ankle instability compared to controls. Clinical Biomechanics, 21(2), 168-174.


Okunuki, T., Koshino, Y., Yamanaka, M., Tsutsumi, K., Igarashi, M., Samukawa, M., & Tohyama, H. (2019). Forefoot and hindfoot kinematics in subjects with medial tibial stress syndrome during walking and running. Journal of Orthopaedic Research, 37(4), 927-932.



Pohl, M. B., Messenger, N., & Buckley, J. G. (2006). Changes in foot and lower limb coupling due to systematic variations in step width. Clinical Biomechanics, 21(2), 175-183.


Schurr, S. A., Marshall, A. N., Resch, J. E., & Saliba, S. A. (2017). Two-dimensional video analysis is comparable to 3D motion capture in lower extremity movement assessment. International Journal of Sports Physical Therapy, 12(2), 163.


Simon, J. E., & Docherty, C. L. (2018). Health-related quality of life is decreased in middle-aged adults with chronic ankle instability. Journal of Science and Medicine in Sport, 21(12), 1206-1209.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



